What is it Periodontal Disease? How does it develop?
Periodontal disease is one of the most common diseases of humans and is responsible for tooth mobility and tooth loss.
Periodontal disease is a contagious, chronic bacterial infection that affects the gum tissue, bone and attachment fibres that support the teeth and hold them in place. Gum disease starts slowly without any pain and may not be apparent until there are serious side effects.
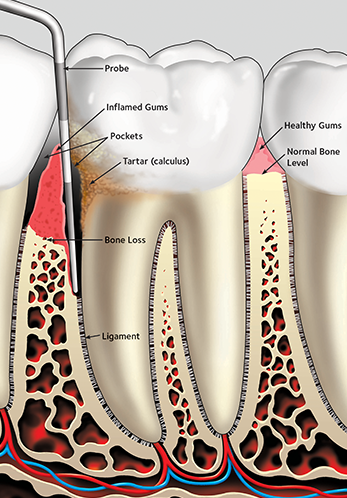
Over time, a build‐up of plaque bacteria (white furry substance) collects at the gum line, eventually hardening on the teeth into calcium deposits called calculus. Brushing and flossing cannot remove calculus. If the calculus is not removed with a professional cleaning, the bacteria can cause inflammation of the gums (gingivitis), penetrate the gum line and finally spread into the underlying bone (periodontitis).
If left untreated, gum disease can result in abscesses or the complete destruction of the tooth’s supporting tissues and, ultimately, tooth loss.
Signs and symptoms
⦁ Bleeding gums when brushing or flossing
⦁ Red, swollen or tender gums
⦁ Receding gums
⦁ Deep pockets
⦁ Metallic taste
⦁ Tooth sensitivity for no apparent reason
⦁ Loose or shifting teeth
⦁ Abscesses, Pus around gums and teeth
⦁ Chronic bad breath
Periodontitis
With time, plaque can spread and grow below the gum line, along the roots of the teeth. If there is more plaque than your body’s immune system can cope with, the infection continues to spread. A space, known as a ‘pocket’, develops between the gum and the tooth, as the socket bone is gradually eroded away. As the disease progresses, the pockets deepen and more gum tissue and bone are destroyed. Often, this destructive process has very few symptoms. However, if untreated, the teeth can become loose and may have to be removed.
Causes and risk factors of Periodontal Disease
Although bacterial plaque build-up is the main cause of periodontal disease, several other factors, including other diseases, medications and oral habits, also can contribute. These factors can increase your risk of gum disease or make it worse once the infection has set in.
⦁ Smoking /vaping/tobacco – worsens periodontal disease and may camouflage the problem by reducing blood supply to the gums. Periodontal disease in smokers occurs 3‐4 times faster than non‐smokers. Apart from causing oral cancer, smoking is one of the biggest reasons for tooth mobility and tooth loss.
⦁ Genetics – research proves that up to 30% of the population may be genetically susceptible to gum disease. Despite aggressive oral care habits, these people may be six times more likely to develop periodontal disease.
⦁ Crowded teeth – due to the difficulty in cleaning effectively.
⦁ Grinding or clenching teeth – The excessive force exerted on the teeth by these habits appears to speed up the breakdown of the periodontal ligament and bone. You may be required to have a custom splint or night guard to reduce the pressure of clenching or grinding on the teeth.
⦁ Poorly controlled diabetes – if you are diabetic, you are at higher risk for developing infections, including periodontal diseases.
⦁ Immune disorders, stress and pregnancy
⦁ Medications – Several types of medications can cause dry mouth, including antidepressants, diuretics and high blood-pressure medications. Without the protection of adequate amounts of saliva, plaque is more likely to form. Other medications may cause the gums to enlarge, which in turn makes them more likely to trap plaque.
How is Periodontal Disease Treated/Managed?
Periodontal disease occurs in a cyclic manner, with bursts of destruction and periods of inactivity. Unfortunately, once destruction of bone occurs the bone does not regenerate and treatment is aimed at preventing any further loss of bone or your teeth.
The success of periodontal treatment is largely due to the effort you as an individual make to remove the daily build‐up of plaque from tooth and gum surfaces. To prevent and help heal inflamed gums, it is essential to control plaque build‐up.
The type of periodontal treatment needed will vary according to the severity of your individual problem.
Periodontal treatment usually involves oral hygiene instruction and removal of plaque and calculus build‐up above and below the gum line.
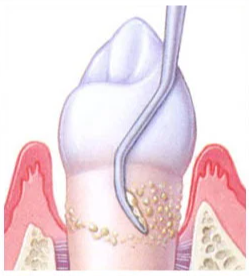
Periodontal debridement involves smoothing the root surfaces to prevent plaque and bacteria reattaching to the tooth.
Regular removal of plaque and calculus (every 3, 6 or 12 months, depending on the situation) is vital to prevent the reoccurrence of periodontal disease. In the most severe of cases, a referral to a Periodontist (Gum Specialist) may be required.
Oral Hygiene Instruction
The first goal is to improve your ability to remove plaque from your teeth. Other home aids may be suggested to help control plaque build‐up, such as mouth rinses and inter‐dental toothbrushes
What are the risks/side effects/complications?
⦁ The gums occasionally feel sore after cleaning, warm salt water mouthwashes will help.
⦁ Your teeth may become more sensitive to hot, cold or sweet substances.
As the gums become healthier, they may shrink or recede. Sometimes spaces may appear between the teeth and the teeth may appear longer. This is due to the elimination of gum inflammation.





